What’s New in the 2025 ACS Guidelines? A Pharmacist-Focused Breakdown
Stay current with the 2025 ACS treatment guideline updates from the American College of Cardiology and American Heart Association. This blog breaks down key changes in pharmacologic strategies, percutaneous coronary intervention (PCI) recommendations, and secondary prevention protocols. Whether you’re in clinical practice, training, or industry, this clear and accessible overview helps you translate the latest evidence into real-world decision-making.
May 26
On February 27, 2025, the American College of Cardiology (ACC) and the American Heart Association (AHA) released the highly anticipated 2025 ACS treatment guidelines, outlining updated recommendations for the pharmacologic and surgical management of acute coronary syndrome. Developed with input from key stakeholders—including the American College of Emergency Physicians (ACEP), the National Association of EMS Physicians (NAEMSP), and the Society for Cardiovascular Angiography and Interventions (SCAI)—this guideline reflects the latest in evidence-based cardiovascular care.
For pharmacists, healthcare trainees, and life sciences professionals, understanding these changes is critical—not only to stay current with evidence-based practices but also to confidently engage in clinical and strategic decision-making.
Before we dive into the updates, let’s revisit what acute coronary syndrome (ACS) actually encompasses—and why these distinctions matter for treatment decisions and patient outcomes.
For pharmacists, healthcare trainees, and life sciences professionals, understanding these changes is critical—not only to stay current with evidence-based practices but also to confidently engage in clinical and strategic decision-making.
Before we dive into the updates, let’s revisit what acute coronary syndrome (ACS) actually encompasses—and why these distinctions matter for treatment decisions and patient outcomes.
Empty space, drag to resize
Overview of Acute Coronary Syndrome
Acute coronary syndrome is one of those cornerstone conditions every clinician needs to recognize and respond to—quickly, clearly, and confidently. For pharmacy professionals, that means not just understanding the clinical terminology, but being able to translate it into real-world medication decisions, collaborative care strategies, and effective patient education. Let’s break it down.
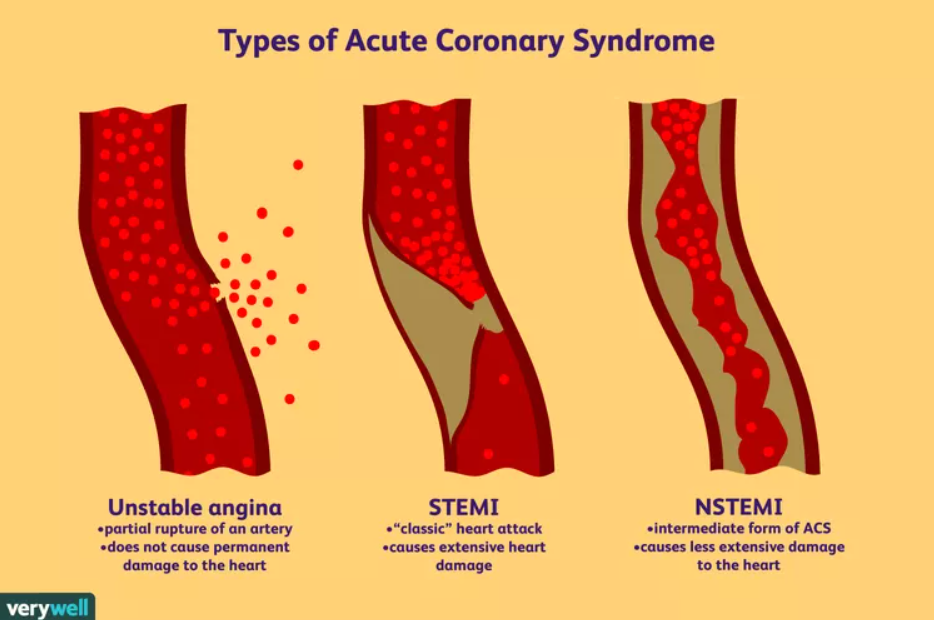
*Sourced from Verywell Health as of April 2025 at https://www.verywellhealth.com/non-st-segment-elevation-myocardial-infarction-nstemi-1746017
As demonstrated in the picture above, acute coronary syndromes are typically caused by the rupture of an atherosclerotic plaque, which leads to partial or complete occlusion of the included vessel. This results in myocardial ischemia and, potentially, myocardial infarction.
Unstable Angina
Unstable angina is characterized by new or worsening chest pain that occurs at rest or with minimal exertion, and it does not result in myocardial necrosis. Unstable angina does not include ST-segment elevation or elevated troponin.
NSTEMI
NSTEMI involves moderate obstruction and the presence of myocardial necrosis, which can be monitored via elevated cardiac biomarkers like troponin. NSTEMI does not include ST-segment elevation on electrocardiography (ECG), which is a major marker for occlusive thromboses.
STEMI
STEMI is what most people know as the common heart attack, presenting with severe occlusion and persistent ST-segment elevation on electrocardiography. STEMI causes significant transmural myocardial necrosis due to complete coronary artery occlusion.
Common symptoms of acute coronary syndrome include difficulty breathing (dyspnea), sweating (diaphoresis), nausea, fainting (syncope), and chest discomfort, which can radiate to the arms, neck, jaw, or back.
Treatment options for acute coronary syndrome vary depending on the diagnosis, though they generally include antiplatelet therapy, anticoagulation, statins, and revascularization procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
Empty space, drag to resize
2025 ACS Guideline Updates: What Clinicians and Pharmacists Need to Know
The 2025 ACS guideline is packed with detailed recommendations—but you don’t need to read the full 200+ pages to understand what’s changed. These nine key takeaways highlight the most impactful updates in acute coronary syndrome treatment, from pharmacologic strategy to procedural best practices. Whether you’re a student, clinician, or working in drug development, staying current on these shifts ensures you’re aligned with today’s clinical standards—and tomorrow’s expectations.
-
Dual antiplatelet therapy (DAPT) is recommended for patients with acute coronary syndrome undergoing percutaneous coronary intervention. Ticagrelor and prasugrel are recommended over clopidogrel to reduce the likelihood of ischemic events (e.g., stent thrombosis).
It is also recommended that patients with non-ST-segment elevation myocardial infarction that are scheduled for an invasive strategy with angiography timing greater than 24 hours receive upstream treatment with clopidogrel or ticagrelor to reduce the risk of major adverse cardiovascular events. In other words, it is recommended to administer a loading dose of clopidogrel or ticagrelor prior to any invasive procedures in these patients. -
Dual antiplatelet therapy with aspirin and an oral P2Y12 inhibitor (i.e., prasugrel, ticagrelor, clopidogrel) is recommended for a minimum of 12 months as the standard approach for patients with acute coronary syndrome who are not at high bleeding risk.
Several strategies may be used to minimize bleeding risk in patients with acute coronary syndrome who have undergone percutaneous coronary intervention and require antiplatelet therapy.- For those at risk of gastrointestinal bleeding, the use of a proton pump inhibitor (e.g., omeprazole, esomeprazole) is recommended
- For patients who have tolerated dual antiplatelet therapy with ticagrelor, de-escalating to ticagrelor monotherapy is recommended at or beyond one-month following percutaneous coronary intervention;
- For patients that require long-term anticoagulation, it is recommended to discontinue aspirin 1 - 4 weeks after percutaneous coronary intervention while continuing a P2Y12 inhibitor—preferably clopidogrel
-
Complete revascularization is recommended for patients with ST-segment elevation myocardial infarction or non–ST-segment elevation acute coronary syndrome. In cases of non-ST-segment elevation acute coronary syndrome with multivessel disease, the decision between coronary artery bypass grafting (CABG) and multivessel percutaneous coronary intervention should be determined by the complexity of the condition and the presence of comorbidities. For STEMI patients, percutaneous coronary intervention of significant nonculprit lesions (obstructions that did not cause the attack) may be performed during the initial procedure or in a staged manner, though a single procedure is preferred. In patients with acute coronary syndrome complicated by cardiogenic shock, urgent revascularization of the causative artery is indicated; however, routine percutaneous coronary intervention of non-infarct-related arteries during the same procedure is not recommended.
-
High-intensity statin therapy is indicated for all patients with acute coronary syndrome, with the option to start ezetimibe at the same time. Patients on maximally tolerated statins that still have a low-density lipoprotein cholesterol (LDL-C) level of ≥70 mg/dL (1.8 mmol/L), should receive an additional nonstatin lipid-lowering agent (e.g., ezetimibe, evolocumab, alirocumab, inclisiran, bempedoic acid). Since patients with acute coronary syndrome are at high-risk for major cardiovascular events, it is also recommended to intensify lipid-lowering therapy if LDL-C levels are between 55 and <70 mg/dL (1.4 to <1.8 mmol/L) despite being on a maximally tolerated statin.
-
Patients with non–ST-segment elevation acute coronary syndrome who are at intermediate or high risk of ischemic events are indicated for an invasive strategy followed by revascularization during hospitalization to lower the risk of major adverse cardiovascular events. For those at low ischemic risk, either a routine or selective invasive approach—guided by further risk assessment—is suggested to help determine the need for revascularization and reduce the likelihood of major cardiovascular complications.
-
Two procedural strategies are recommended for patients with acute coronary syndrome who are undergoing percutaneous coronary intervention:
- The radial artery approach is preferred over the femoral approach to minimize the risks of bleeding, vascular complications, and death;
- Intracoronary imaging is recommended to guide percutaneous coronary intervention in patients with acute coronary syndrome who have complex coronary lesions. Intracoronary imaging allows for a more detailed visualization during procedures to optimize stent placement, assess lesion severity, and thus improve clinical outcomes.
-
Clinical trial evidence supports the use of a microaxial flow pump in select patients with cardiogenic shock related to acute myocardial infarction to aid in proper blood flow and reduce mortality. Despite this, the pump is associated with a higher risk of complications like bleeding, limb ischemia, and kidney injury when compared to standard care. With this, careful monitoring of vascular access and weaning of support is crucial to appropriately balance the benefits and risks of using a microaxial flow pump.
-
Maintaining a hemoglobin level of 10 g/dL through red blood cell transfusion may be reasonable for patients with acute coronary syndrome and either acute or chronic anemia who are not experiencing active bleeding.
-
Following hospital discharge, it is essential to prioritize secondary prevention. A fasting lipid panel should be obtained 4-8 weeks after starting or modifying lipid-lowering therapy. It is recommended to refer patients for cardiac rehabilitation as well, with home-based programs available for those who are unable or prefer not to attend in-person sessions.
These updates reflect more than just evolving clinical preferences—they signal a deeper shift toward precision-based care in cardiology. For pharmacists, healthcare professionals, and industry innovators alike, staying fluent in guideline changes like these isn’t just helpful—it’s essential. Whether you're optimizing therapy at the bedside or strategizing product development upstream, these insights are the foundation of safe, evidence-based, patient-centered care.
Why This Matters—for Clinicians, Pharmacists, and Industry Professionals
Each year, more than 800,000 people in the U.S. experience a heart attack, highlighting the urgency of effective, up-to-date acute coronary syndrome treatment. As Dr. Sunil V. Rao, Chair of the 2025 guideline writing committee, emphasized: “Patients with ACS are at the highest risk for cardiovascular complications both acutely and chronically, which emphasizes the importance of staying up to date on the most recent evidence.”
For healthcare professionals across practice and industry, these updates are more than clinical housekeeping—they're a roadmap for improving outcomes, preventing complications, and making better-informed decisions at every stage of care.
The 2025 ACS guidelines underscore meaningful shifts in acute coronary syndrome care—from intensified lipid management to evolving PCI strategies and secondary prevention frameworks. These changes reflect not only the latest evidence, but the growing need for strategic, patient-centered decision-making at every level of care.
The 2025 ACS guidelines underscore meaningful shifts in acute coronary syndrome care—from intensified lipid management to evolving PCI strategies and secondary prevention frameworks. These changes reflect not only the latest evidence, but the growing need for strategic, patient-centered decision-making at every level of care.
At Ceuticon, we’re committed to equipping student pharmacists, working professionals, and healthcare innovators with insights that matter. By translating updates like these into clear, actionable takeaways, we help our community lead with confidence—and contribute to better outcomes across the healthcare ecosystem.